* I am not a doctor and am only sharing my experience, I am also working with a doctor and have had labs run, please work with a doctor if you suspect something similar *
I wanted to share my experience with thyroid supplementation and low cortisol. My oral waking and midday temperatures were sitting around 97F and 97.5F respectively. As an aside, my axillary is always 0.5-1F warmer, yes warmer, than my oral temperature. I think what I am about to describe could have a part in that but I am unsure of the mechanism yet. My oral temperature has been in the low 96F but lifestyle interventions, supplements, and some topical thyroid were able to increase it.
I was taking 6ug T4 and 3ug T3 on waking and before bed, plus 8ug T3 only around midday, in my navel. Having done some research on T3 monotherapy, I decided to give the experiment a try due to high revT3, still high tsh, low temperatures, etc. I did 1 drop of the 8ug T3 on my navel upon waking, midday, and before bed. This exposed a low cortisol or improper cortisol response – for example, I may have had sufficient cortisol but due to cortisol binding globulin, an issue at the receptor level, etc. the response wasn’t adequate. This brought on days of blood glucose regulation issues, a decreased desire to eat, diarrhea, a wired but tired feeling, insomnia, blood pressure regulation issues, achy feeling around my kidney/ adrenal area, a mild cough, drop in body temperature, shivers, achy feeling around my sternum, achy feeling around my thyroid and the anterior cervical nodes, feeling strung out like I just had some coffee, frequent urination, body water swings (I sit around 116lbs but swung up to 121lbs then down to 114.6lbs over 2 days), achy muscles not recovering as they normally do from my workout, brain fog, and a general unwell feeling. I stopped the thyroid cold turkey, which arguably was not the best idea, but if it was pushing my adrenal glands harder than they could function, continue to stress them does not follow. I also figured this would be safe given I took the doses topically and was not taking even 1 grain of thyroid.
What I am grateful for about this experience, is the response elucidated many of my prior health issues. Low cortisol is implicated in: allergies – I used to have really bad MCAS; postural orthostatic tachycardia syndrome (POTs) – all the salt cravings, graying out upon standing, lower blood pressure in general, etc.; hypoglycemia – I had ketotic hypoglycemia and the ketotic part was basically non-existent due to supplementing vitamins B2 and B5 (B5 is especially important for the adrenals), and ALCAR+allicin (for possible TMAO issues), now I usually only have issues with hypoglycemia near my period and given the progesterone drop and cortisol’s relationship to estrogen, this makes more sense; recurring rhabdomyolysis – this can be due to too low or too high cortisol; hypermobility/ hEDS – including thin skin and bruising; anxiety; insomnia; night sweats; frequent colds; inability to handle stress – almost craving the stress to feel normal; some hyperpigmentation; freezing hands, feet, nose, and butt; etc. What I find truly crazy is I used to live my life with this strung out, on edge feeling 24/7, the type A, go-go-go personality, then I would crash and sleep for a few days and repeat the process.
I am recovering with Thorne’s adrenal cortex, pantethine (vitamin B5), salt in tangerine juice, sun and grounding for the SCN, trying to relax as much as possible, licorice tea topically, and continuing to eat sufficient protein and nutrient dense food even though I feel nauseous, etc.
Resources
Effects of pantothenic acid supplementation on adrenal steroid secretion from male rats: https://pubmed.ncbi.nlm.nih.gov/18520055/
Vitamin B5 and hypotension: https://altmedrev.com/wp-content/uploads/2019/02/v16-3-263.pdf
Low levels of skin cortisol leads to acne (many thing can as well like vitamin B5 deficiency): https://www.acne.org/what-is-cortisol-and-does-it-affect-acne.html
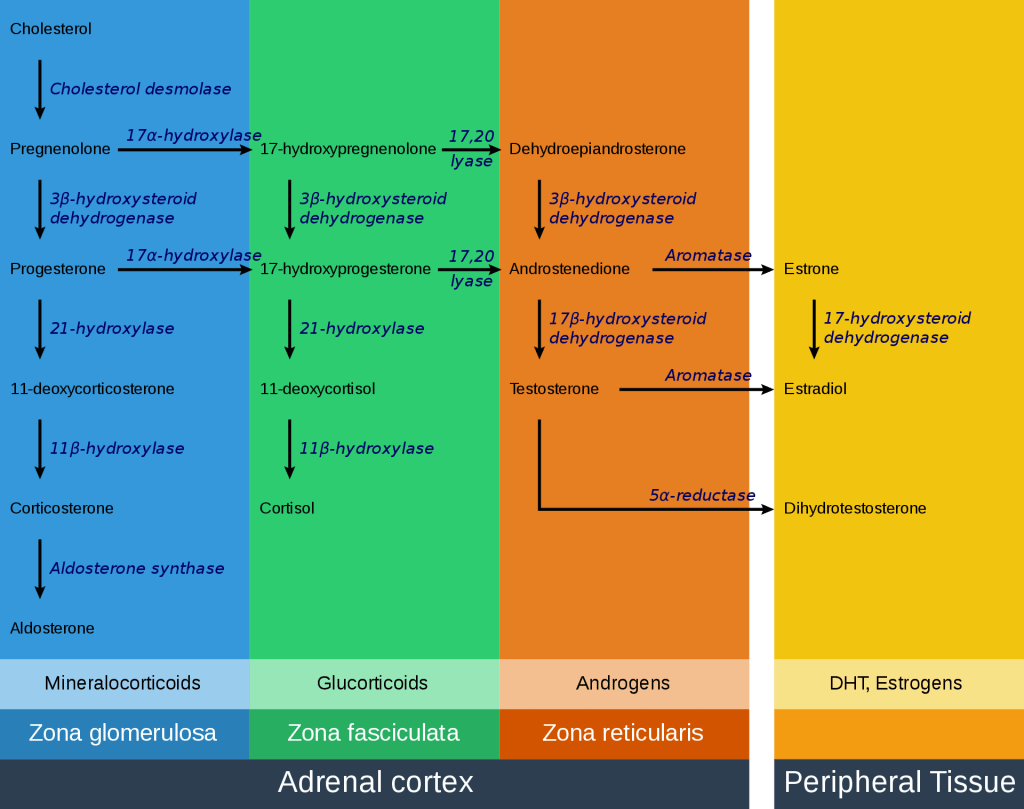
https://upload.wikimedia.org/wikipedia/commons/a/a6/Adrenal_Steroids_Pathways_-_edited.svg
High estrogen levels increase cortisol binding globulin, making cortisol inactive: https://anabolicminds.com/community/threads/cortisol-and-estrogen-relationship.59334/
Stop the thyroid madness has a lot of information on the thyroid-aldosterone-cortisol relationship